A 2011 report commissioned by the German Medical Association (BÄK) found that, despite there being no clear legal authority to do so, over half of German doctors (88% of those practising in Bavaria) have sent patients home with prescriptions for placebo drugs.
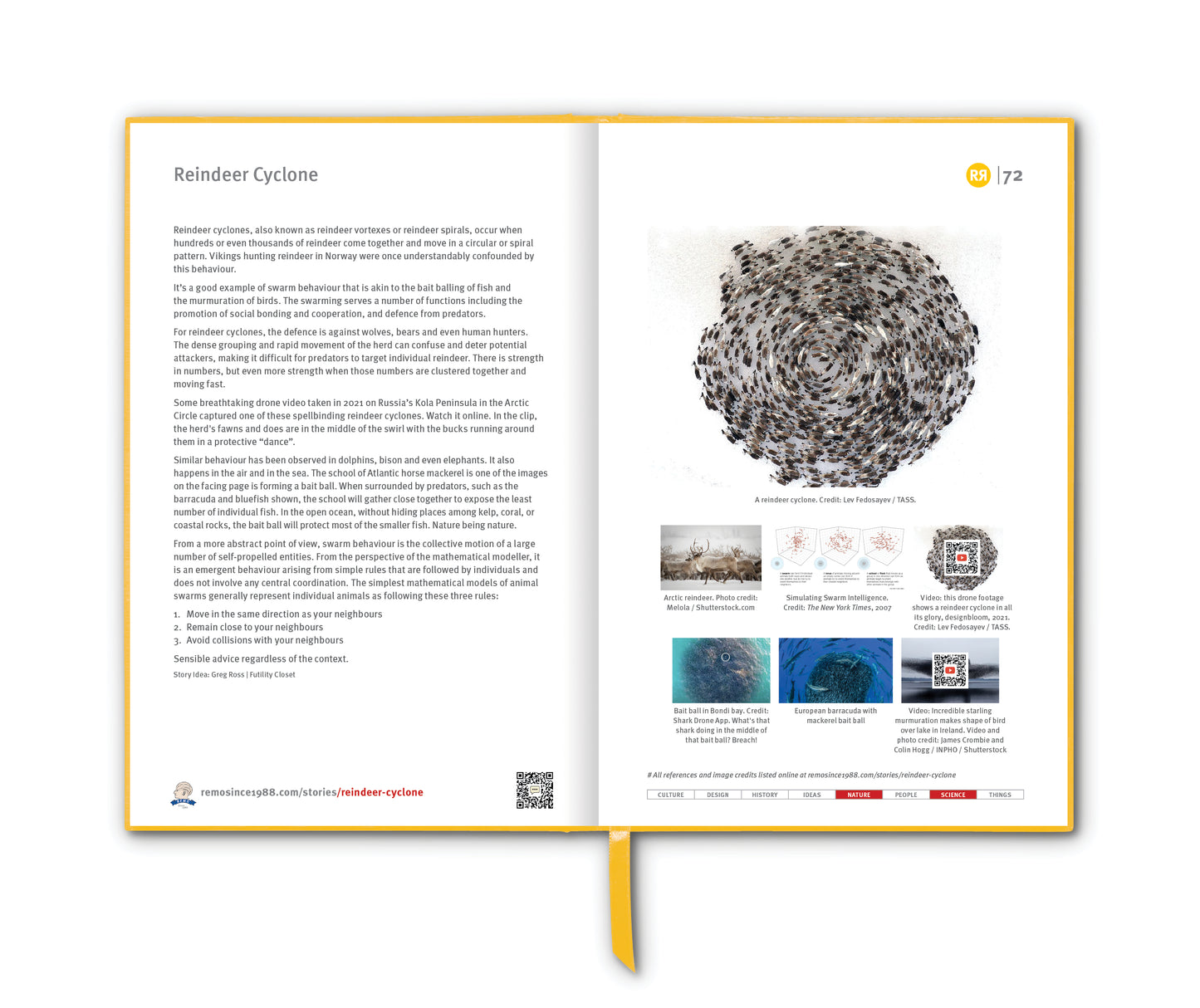
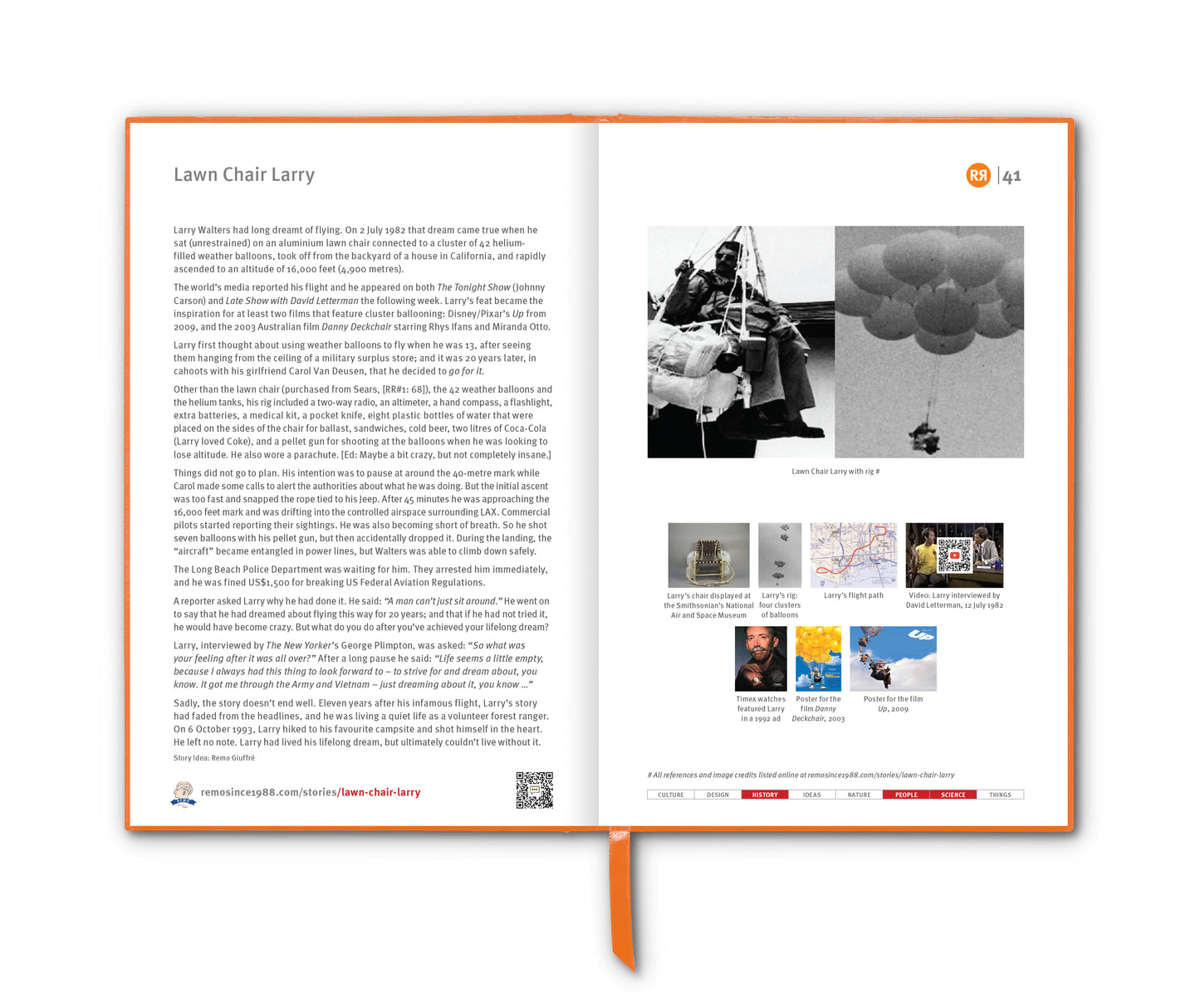
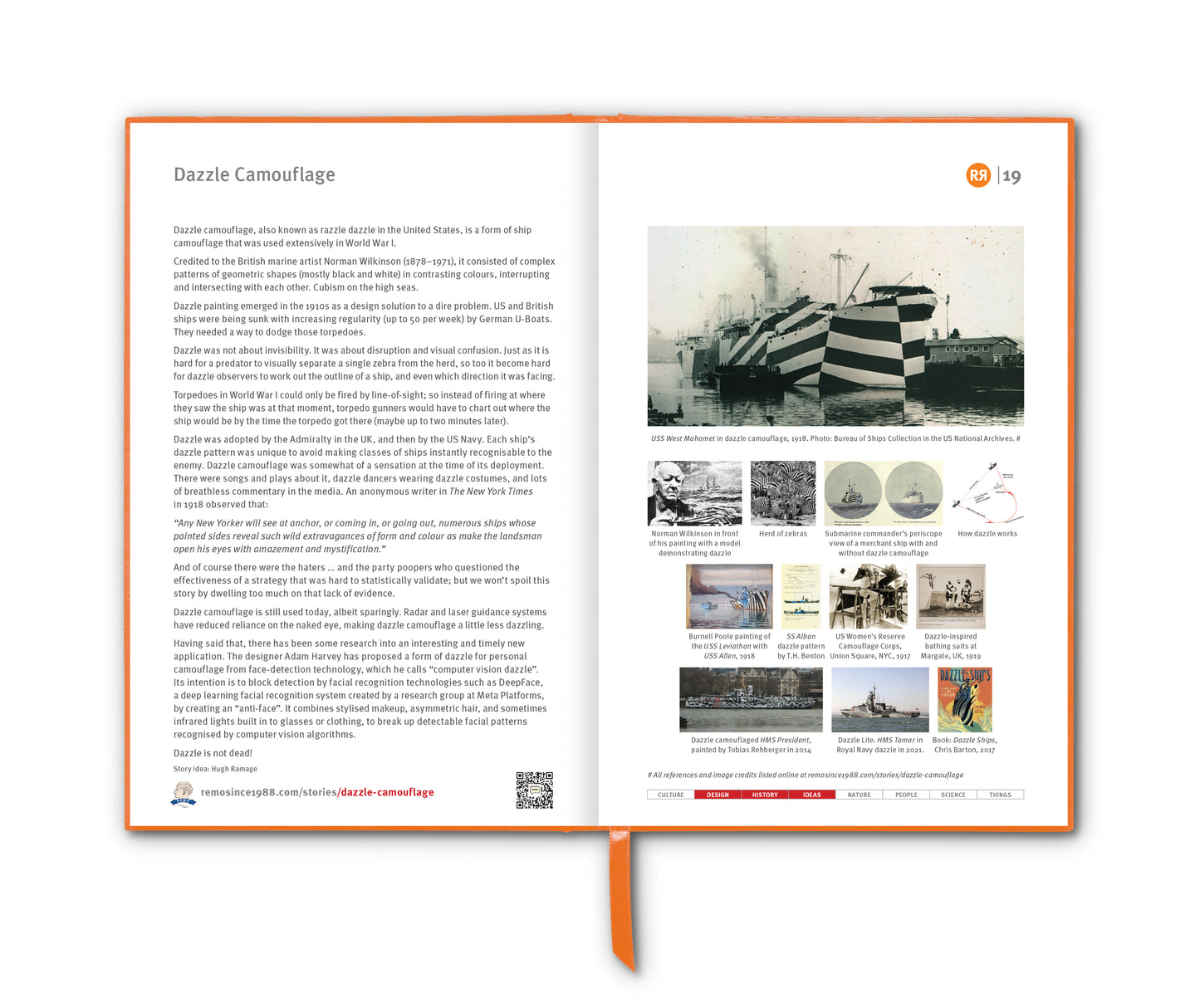
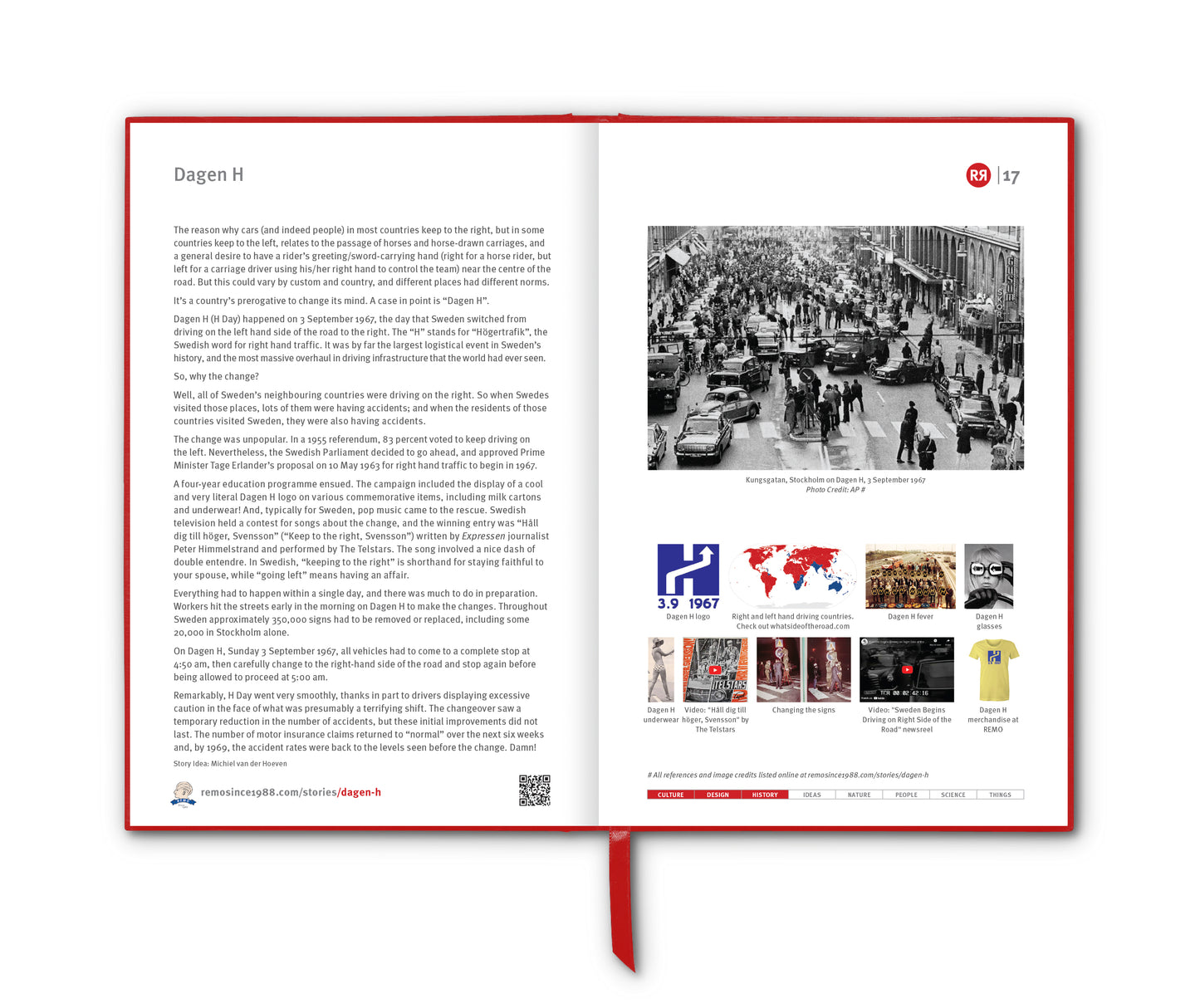
A placebo can be roughly defined as a sham medical treatment, e.g. sugar pills, saline injections, sham surgeries and other procedures. The term placebo, from the Latin “I shall please” was first used in a medical context in the 18th century, but the principle behind it is much older. Healers and physicians throughout history have recognised that patients often improve simply because they believe they are being treated.
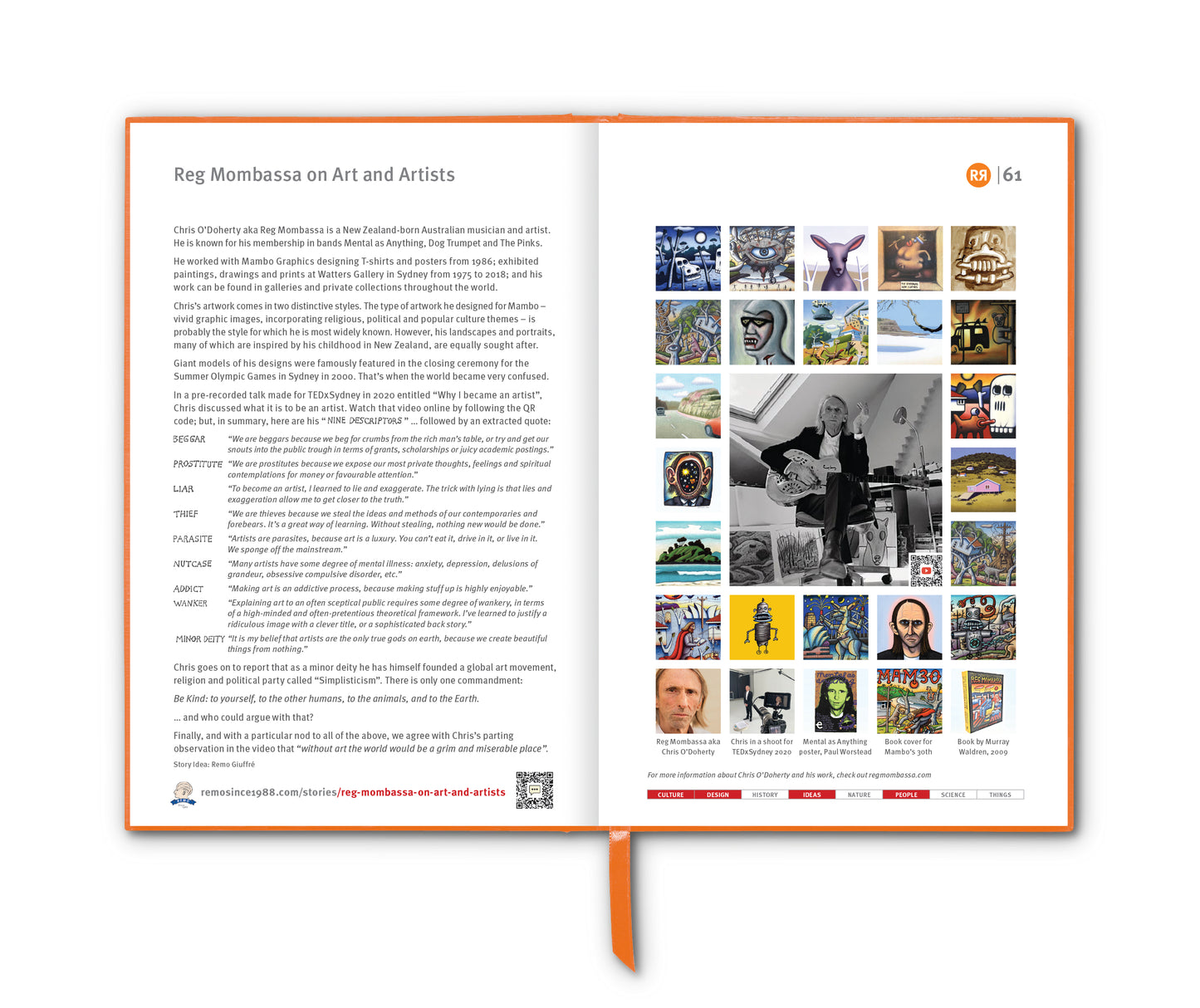
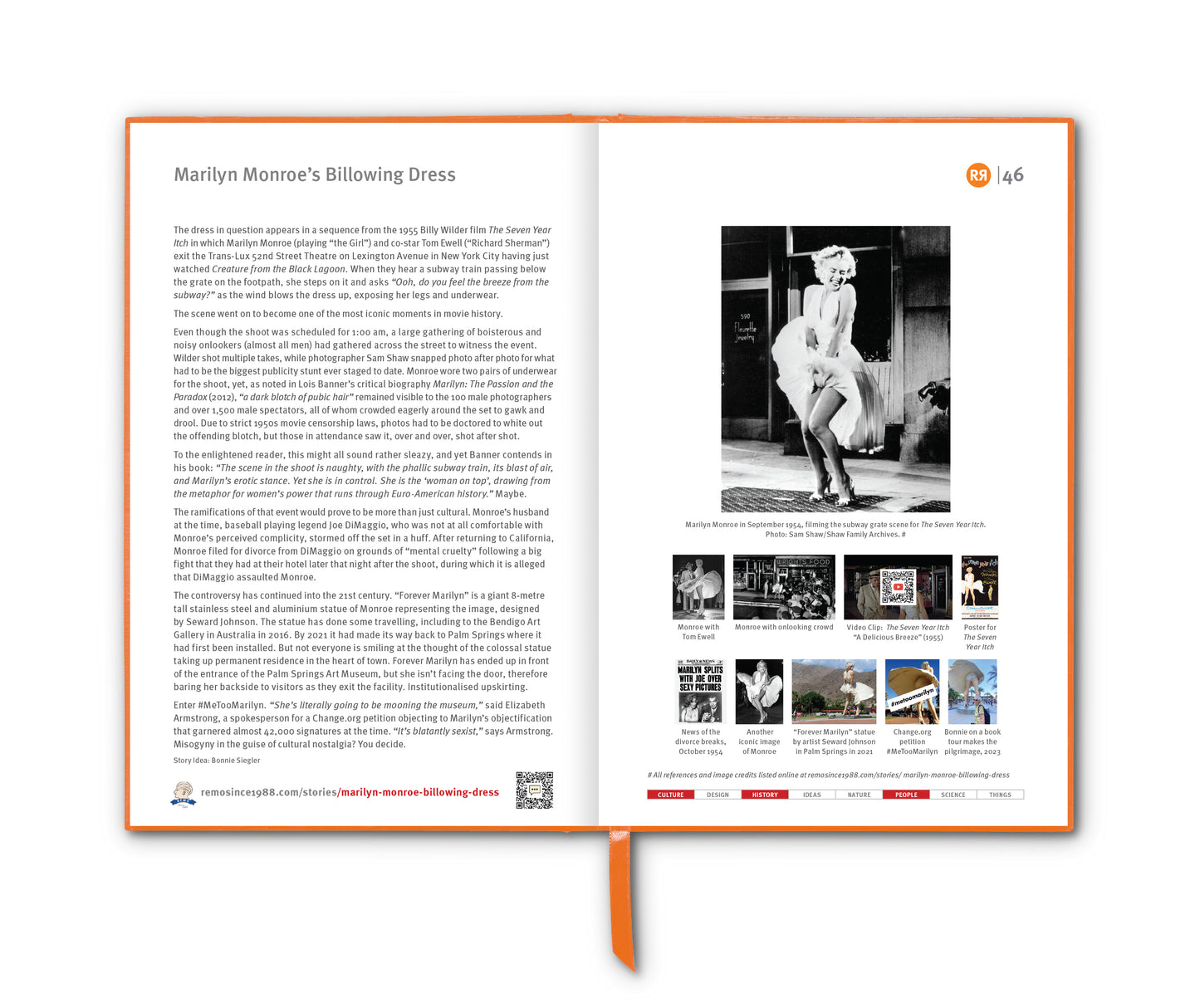
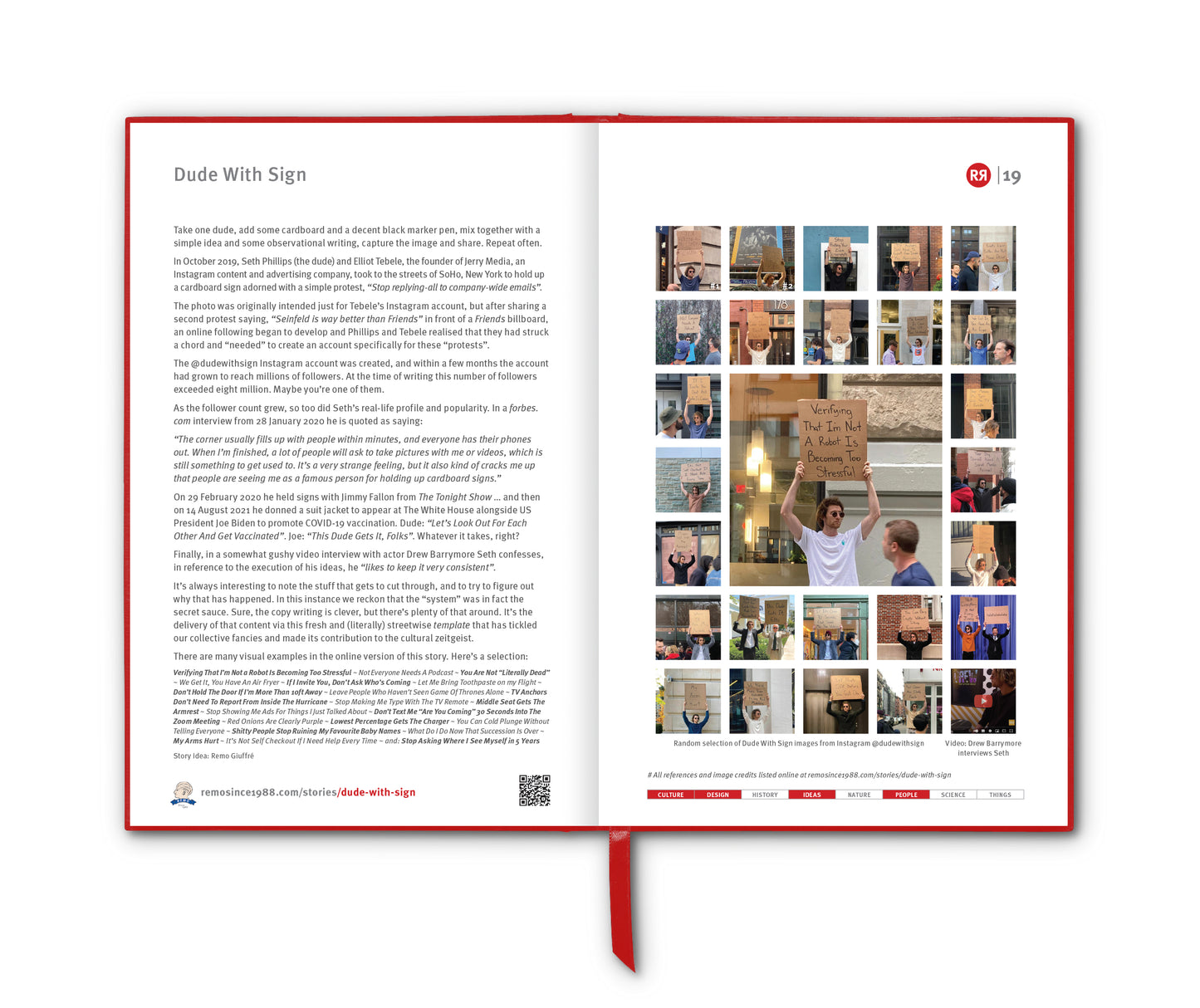
In ancient times, the line between ritual and remedy was blurred. Egyptian priests, Greek physicians, and medieval healers all relied on faith as much as medicine. The Greek physician Hippocrates noted that a patient’s trust in their physician could be a decisive factor in recovery. For centuries, medicine and magic overlapped, and healing often depended as much on expectation as on herbs or instruments. But it was during the rise of scientific medicine that the placebo began to be studied systematically.
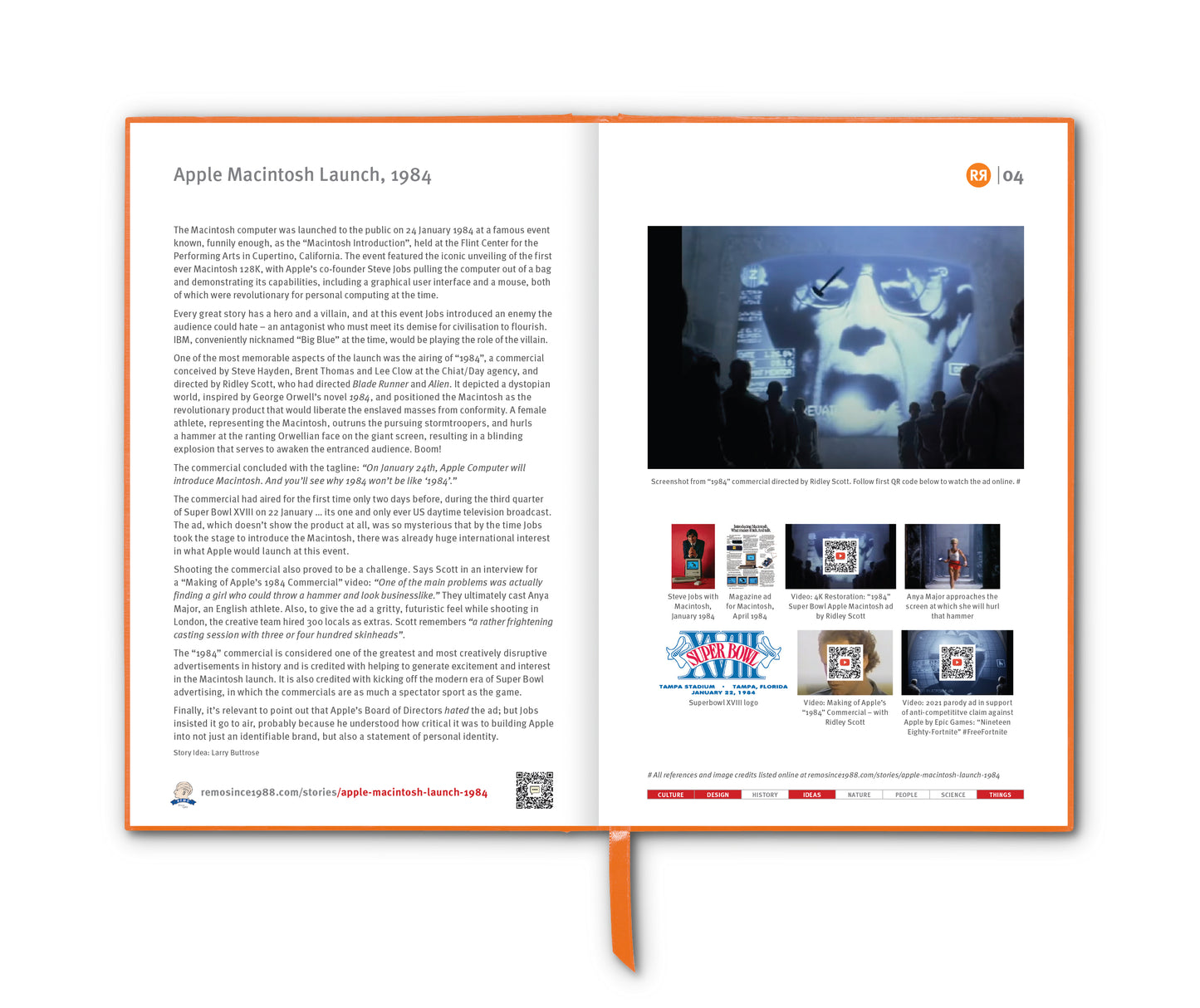
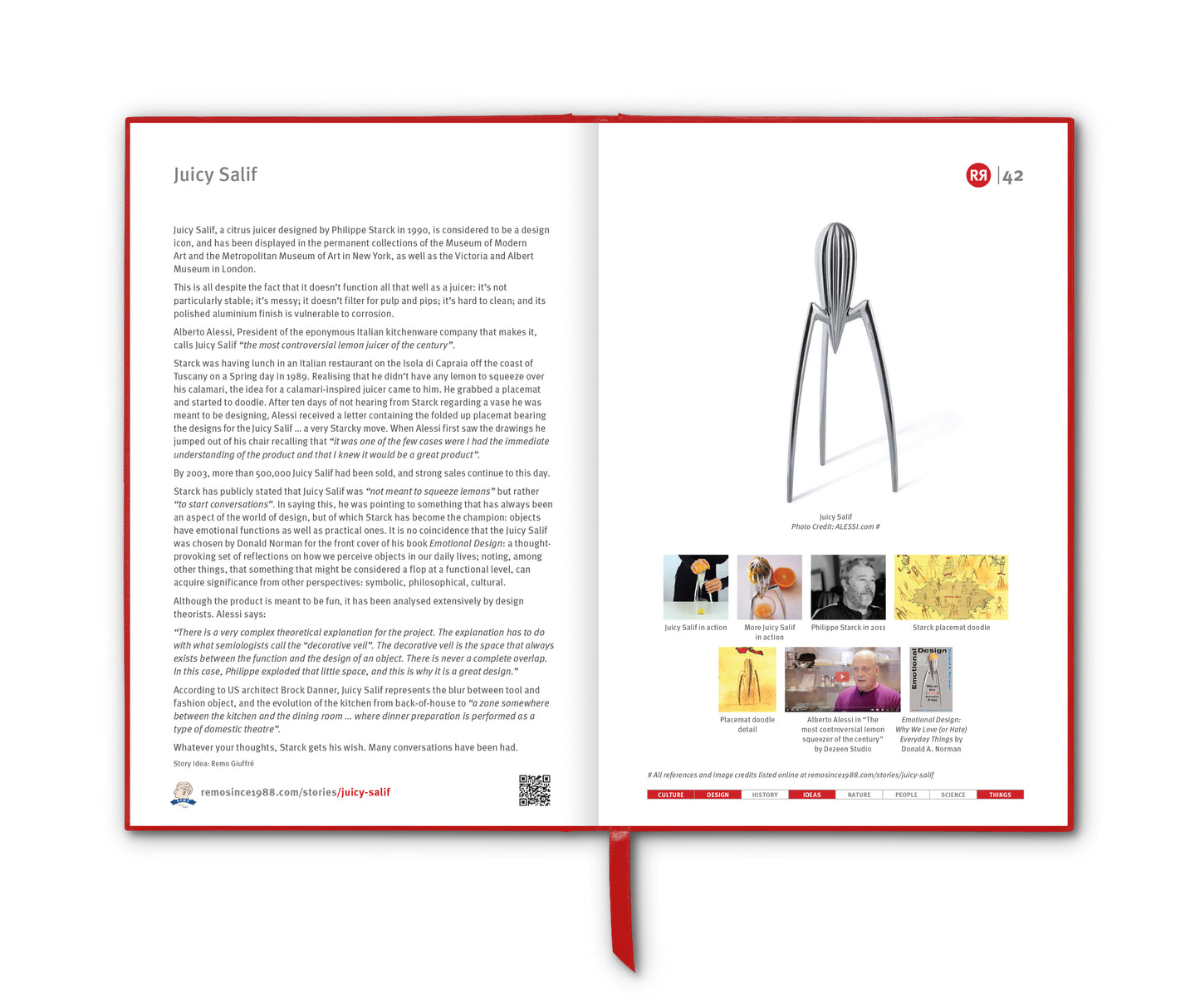
The turning point came during World War II, when American anaesthetist Henry K. Beecher found himself treating soldiers in Italy with dwindling supplies of morphine. In desperation, a nurse injected a wounded man with saline, telling him it was a painkiller. The soldier’s agony eased – not because of chemistry, but because of belief. Beecher later explored this idea in his 1955 paper “The Powerful Placebo”, arguing that up to a third of medical outcomes could be explained by patients’ expectations alone. His claim captured imaginations and helped shape the modern clinical trial: the randomised, double-blind, placebo-controlled study – now the gold standard for testing new treatments.
Over the following decades, remarkable placebo stories emerged. In the 1950s, surgeons studying angina performed “sham operations”, making incisions but performing no actual surgery. Many patients still reported dramatic improvement. Placebo pills for depression, injections for Parkinson’s disease, and even inert capsules for chronic pain all seemed to work under the right psychological conditions. Colour and form mattered too – red pills were seen as energising, blue as calming; branded tablets as more trustworthy than generics.
Yet, as the placebo’s reputation grew, so too did skepticism. When researchers revisited Beecher’s conclusions with modern statistical rigour, they found flaws. Many of his studies lacked proper controls, and patients might have improved naturally over time or reported feeling better simply to please their doctors. A major review published in 2001 by Danish researchers Asbjørn Hróbjartsson and Peter Gøtzsche concluded that, compared with no treatment at all, placebos had little measurable effect on objective medical outcomes. In other words, the placebo effect might be powerful in perception – but limited in physiology.
Still, modern neuroscience has shown that expectation can measurably alter brain chemistry. Placebos can trigger the release of endorphins and dopamine, modulating how pain and pleasure are experienced. They can’t cure infections or shrink tumours, but they can meaningfully change how illness feels – and that matters. The patient’s trust, the healer’s authority, the ritual of care itself – these combine to create real, observable changes in the experience of sickness and relief.
___________________________
References
sites.harvard.edu/sitn/2016/09/14/just-sugar-pill-placebo-effect-real
smh.com.au/healthcare/five-myths-about-placebos
theguardian.com/science/2011/mar/06/half-german-doctors-prescribe-placebos
sciencedirect.com/science/article/abs/pii/S0895435697002035
theconversation.com/the-fascinating-story-of-placebos-and-why-doctors-should-use-them-more-often
Images
1. happy capsuls. Photo by amjd rdwan on Unsplash
2. Engraved bust of Hippocrates, 1881
3. A quack treating a patient with placebo Perkins Patent Tractors, James Gillray, 1801
4. Dr Henry Beecher, 1975. Photo credit: Yousuf Karsh
5. Army-issued morphine syrettes used in WW2
6. Placebo effect diagram. Credit: sitn.hms.harvard.edu